George Crawford, MD
Inguinal Hernia Repair Open
Procedure Overview
Inguinal hernias can be categorized as direct, indirect, femoral.
Inguinal Hernia repair techniques fall under two categories: Tension and Tension Free.
Tension techniques suture the anterior abdominal walls or other structures together to recreate the inguinal canal. They are usually performed using an open procedure. This technique is often used where infection is a concern.
Tension free open repair options with mesh include Plug & Patch, Lichtenstein and Bilayer Connected Mesh Device.
INDICATIONS:
- The existence of an inguinal hernia has traditionally been considered sufficient reason for operative intervention.
- Surgical repair is recommended electively to avoid incarceration or strangulation. NOTE: reducible inguinal hernias can be safely observed in the elderly population with a sedentary lifestyle or high morbidity for surgery.
- Inguinal hernia repair has no absolute contraindications
(Back to the top)

Pre-operative Patient Care
Typical recommendations for pre-operative care may include, but are not limited to, any of the following:
- CT Scan is recommended for complicated, large, questionable, or recurrent hernias.
- Nothing by mouth (NPO) for 8 hours before surgery.
- Cardiopulmonary evaluation as needed.
- Anesthesiology consultation as needed.
Prophylactic antibiotics for patients with high risk of infection. (Although preoperative antibiotics are recommended by many surgeons, their benefit in patients with uncomplicated hernias has not been established).
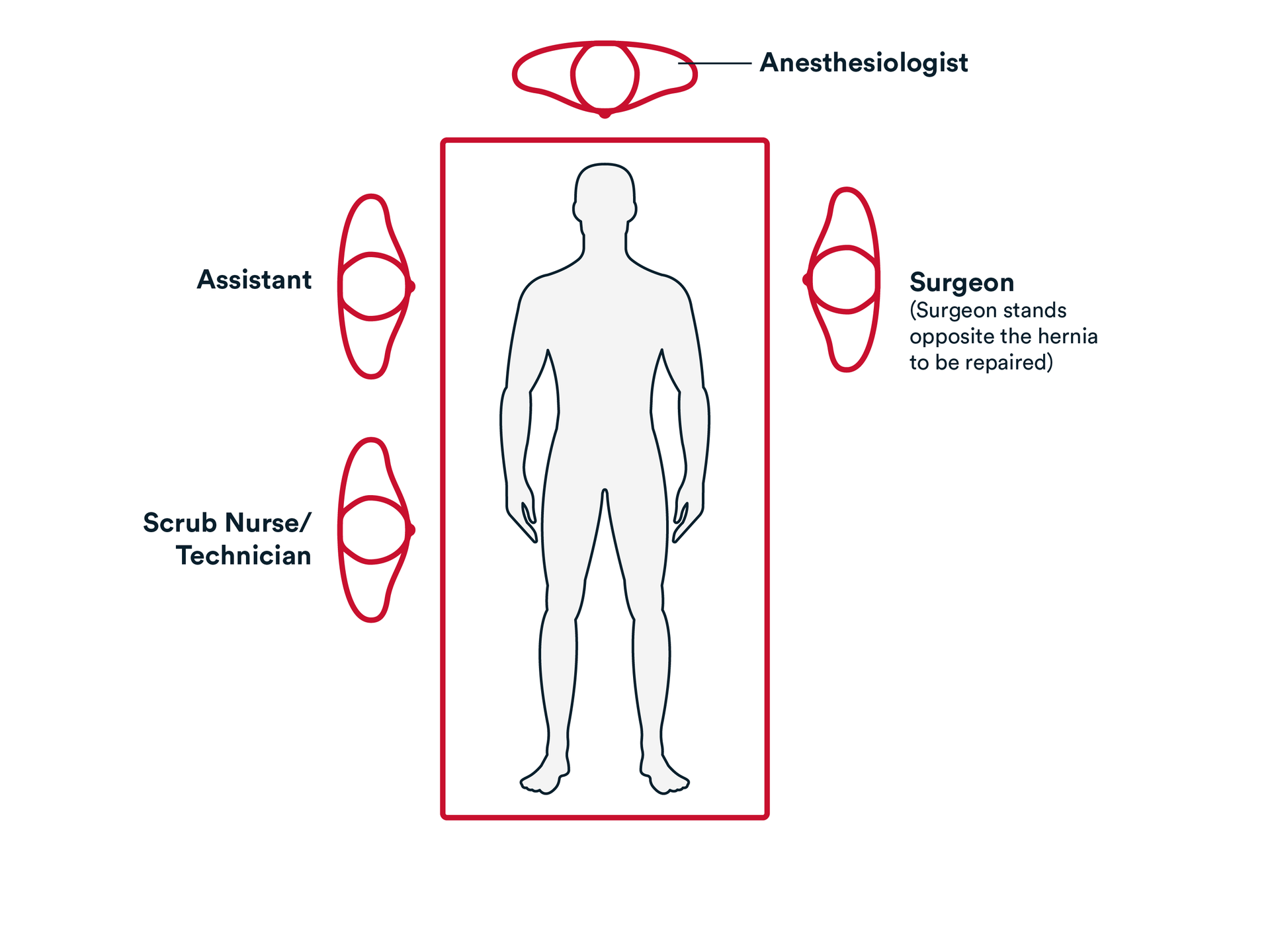
Prep & Patient Positioning
Common patient positioning:
- Open approach: The patient is positioned supine on the operating table. The correct surgical site is clipped free of hair and prepped in the standard sterile fashion.
Operative Steps
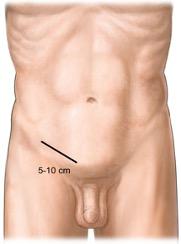
1. Access
- Generally, an incision is made over the inguinal canal, and it is carried down through the subcutaneous tissues.
- Scarpa’s fascia is then identified and incised. If needed, hemostasis may be obtained using electrocautery.
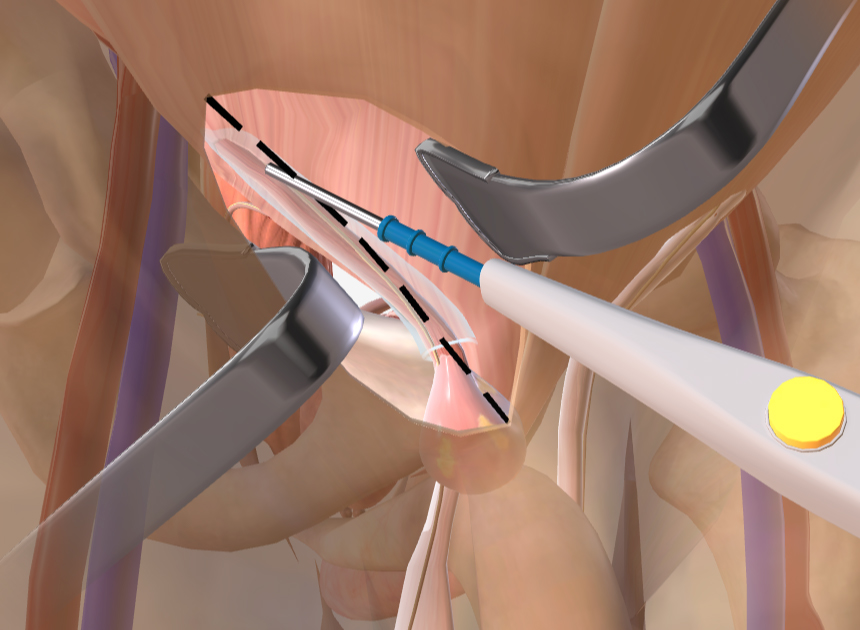
- The external oblique is identified. Typically, a small incision is made in the external oblique, and the Facia is separated and opened towards the external inguinal ring.
- The external oblique is generally retracted laterally to expose the inguinal canal, as well as the cord structures.
- The cord structures are dissected away from the pubic tubercle. Commonly, a Penrose drain is placed around the cord structures for retraction.
- Dissection on the cord structures is typically performed mediately to laterally to identify the indirect hernia sac.
2. Repair
- If present, the indirect hernia sac is dissected away from the cord structures, and then suture ligated.
- The distal hernia sac is removed.
- Cord lipomas are removed, using suture, ligation and electrocautery.
- A mesh such as an ULTRAPRO™ Hernia System is placed in the internal inguinal ring and secured in place using interrupted technique with size 0 or 2-0 suture such as PROLENE™ Polypropylene.
- Generally, attention is turned to the inguinal canal floor. A weakness of the floor can be repaired by securing the mesh of choice in place along the shelving edge of the inguinal ligament and the conjoined tendon.
- If necessary, a suture may be used to re-create the internal inguinal ring.
3. Closure
- A size 0 suture, such as Coated VICRYL™ Plus Antibacterial suture is generally used to re-approximate the external oblique fascia in a running fashion.
- Size 3-0- suture, such as Coated VICRYL™ Plus Antibacterial suture is used to re-approximate Scarpa’s Fascia.
The wounds are closed using synthetic absorbable suture, such as MONOCRYL™ Plus Antibacterial suture, and a topical skin adhesive such as DERMABOND™ Mini Topical Skin Adhesive, or any appropriate dressing.
Post-operative Patient Care
Typical recommendations for post-operative care may include, but are not limited to, any of the following:
- The patient is out of bed, ambulating, with appropriate pain control.
- Diet is advanced as tolerated, with plans for discharge on postoperative day 0 for routine umbilical hernia.
- Lift nothing heavier than 25 lbs. for two weeks.
- Resumption of normal activity, minus lifting restrictions, occurs within 1 day following the procedure.
- Discharge instructions consist of pain management, instructions on the future signs and symptoms indicating potential complications (see below), and an office appointment in 1 weeks’ time.
Potential complications may include but are not limited to, any of the following:
- Nausea, vomiting, or severe coughing spells.
- Fever greater than 101.5 degrees.
- Redness or Erythema.
- Swelling or drainage from the previous hernia site.
- Change in amount of drainage or the color of the drain output if a drain is present.
Additional resources

Access our on-demand Hernia video library
Looking for more? Explore procedural videos and webinars from global experts
HERNIAcademy
Offering comprehensive education about the treatment of inguinal and abdominal hernias