Operative Steps
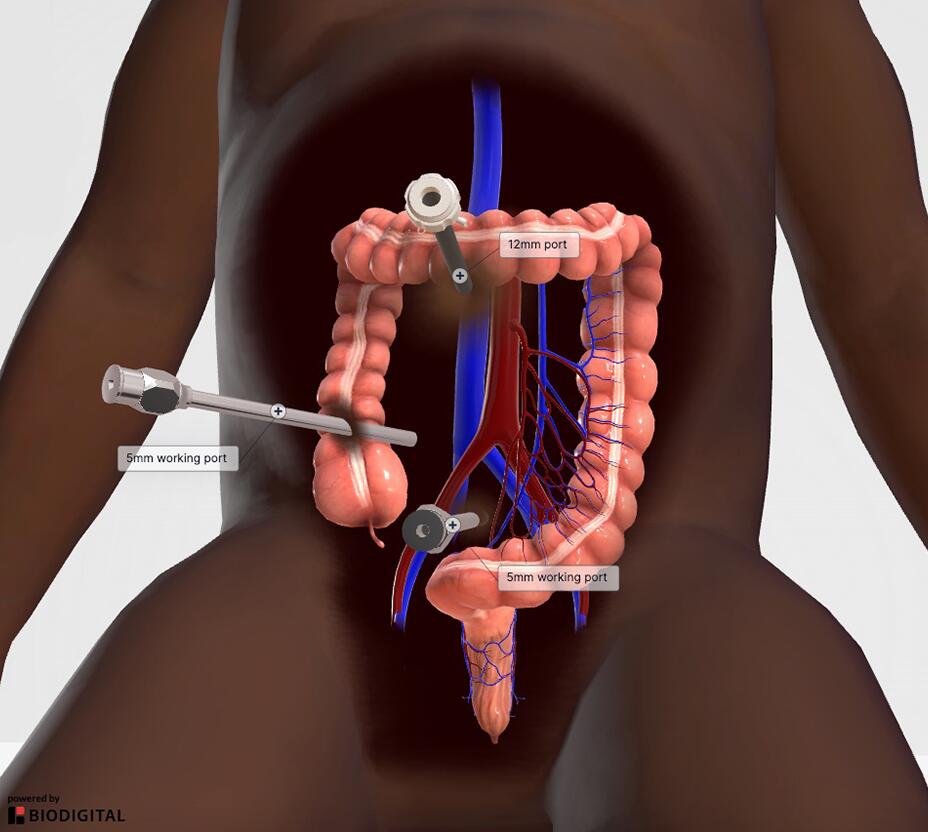
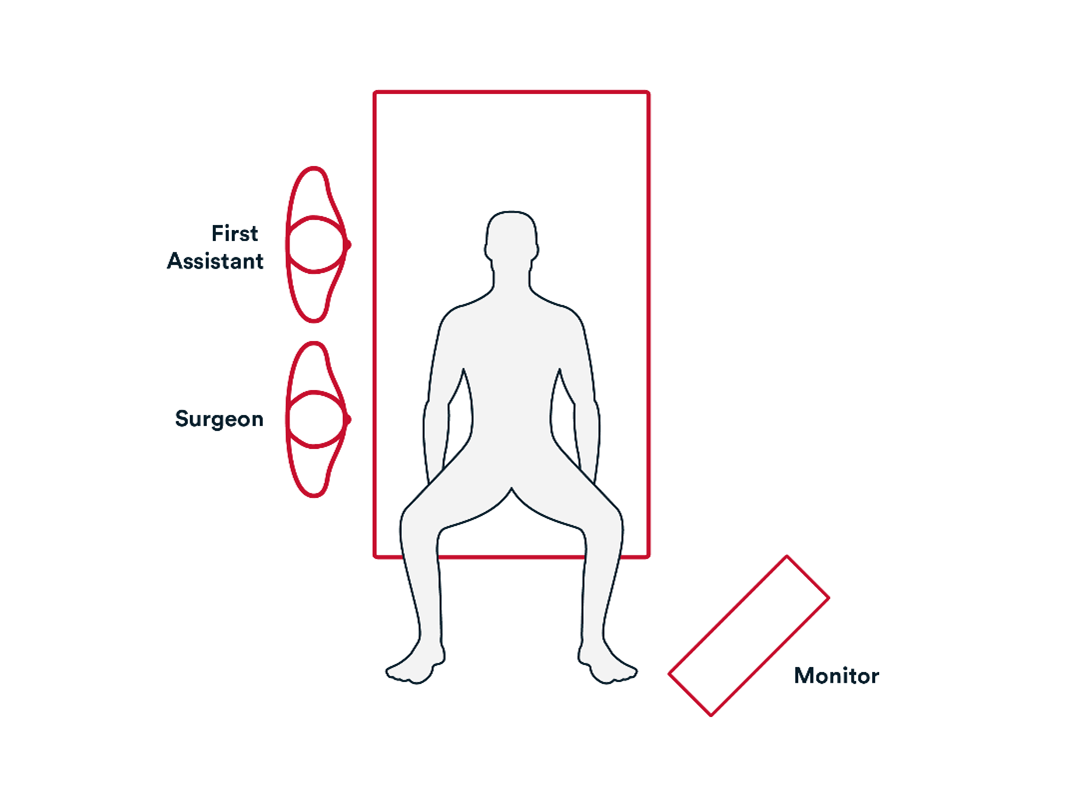
1. Access
- Initial Access to the abdomen is generally obtained by either:
- Veress needle technique.
- Direct trocar view technique.
- Explore the abdominal cavity.
- Take down any adhesions.
2. Repair
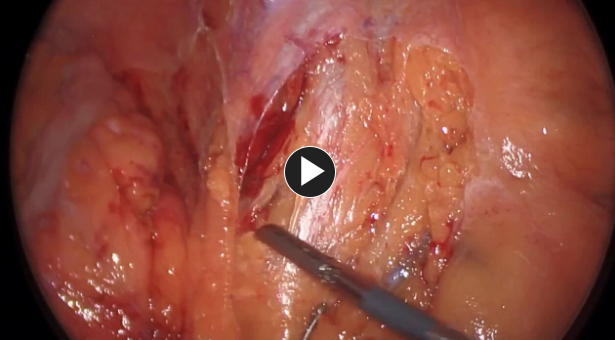
- Access and divide inferior mesenteric artery after identifying the left ureter.
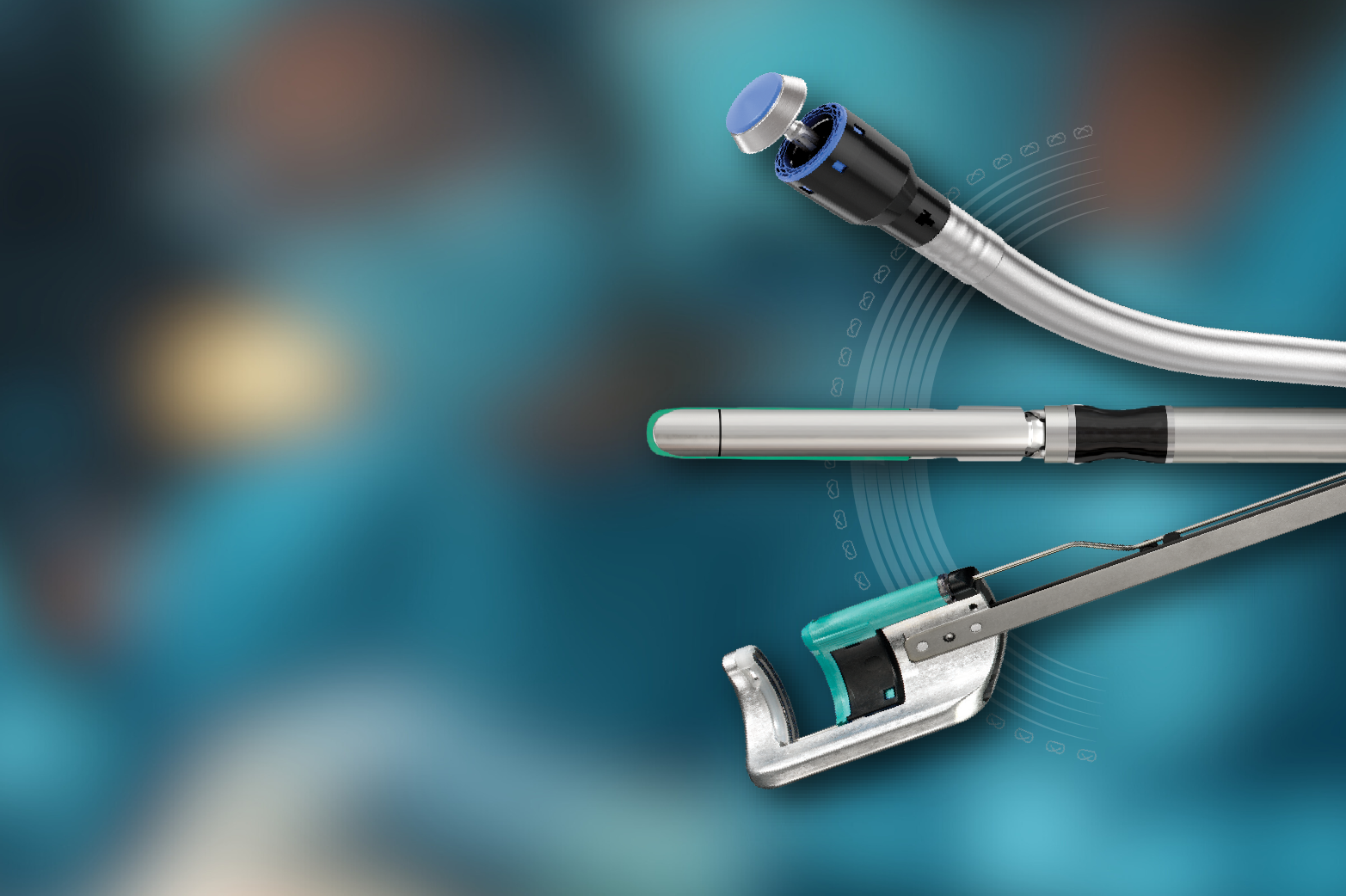
- Mobilize the descending colon and splenic flexure with an energy device such as ENSEAL™ X1 Curved Jaw Tissue Sealer.
- Transect the proximal sigmoid colon using a stapling device, such as ECHELON™ 3000 Stapler and remove specimen.
- Subcuticular layer and skin are closed using synthetic absorbable monofilament, such as Monocryl™ Plus Antibacterial suture, and any appropriate dressing.
Potential complications include but are not limited to:
- Surgical bleeding
- Staple line Leak
- Wound infection
- Ileus
Additional resources