Nezar Jrebi, MD and Jay Redan, MD
Laparoscopic Right Hemicolectomy

Procedure Overview
Laparoscopic right hemicolectomy is one type of partial colectomy that involves removal of the terminal ileum to the mid-transverse colon. When performed for malignant disease an envelope of mesentery together with the corresponding lymphatic drainage with high ligation of supplying artery, this technique called Complete Mesocolic Excision (CME) followed by anastomoses to reestablish bowel continuity.
INDICATIONS:
- Colon cancer
- Unresectable polyps
- GI bleeding
- Inflammatory bowel disease
- Cecal Volvulus
- Diverticulitis
- Ischemic Colitis
- Intestinal Obstruction
- Appendiceal Tumor
- Neuroendocrine Tumor

Pre-operative Patient Care
Typical recommendations for pre-operative care may include, but are not limited to, any of the following:
- Cardiac evaluation
- Pulmonary evaluation
- Prehabilitation before surgery as indicated (such as diabetic control (A1c), stop smoking, weight loss)
- Mechanical bowel prep and oral antibiotic
- Optimize nutrition
- Carbohydrate load except for diabetic patient
Prep & Patient Positioning
Common patient positioning:
- Typically, the patient is placed in the supine or lithotomy position, depending on surgeon preference.
- Arms tucked.
- IMPORTANT: Patient secured to the table.
- OG (oral-gastric) tube.
- Venous compression boots.
- Foley catheter.
- Sometimes surgeon will go between the legs for the transverse colon part of the operation to maintain good ergonomics.
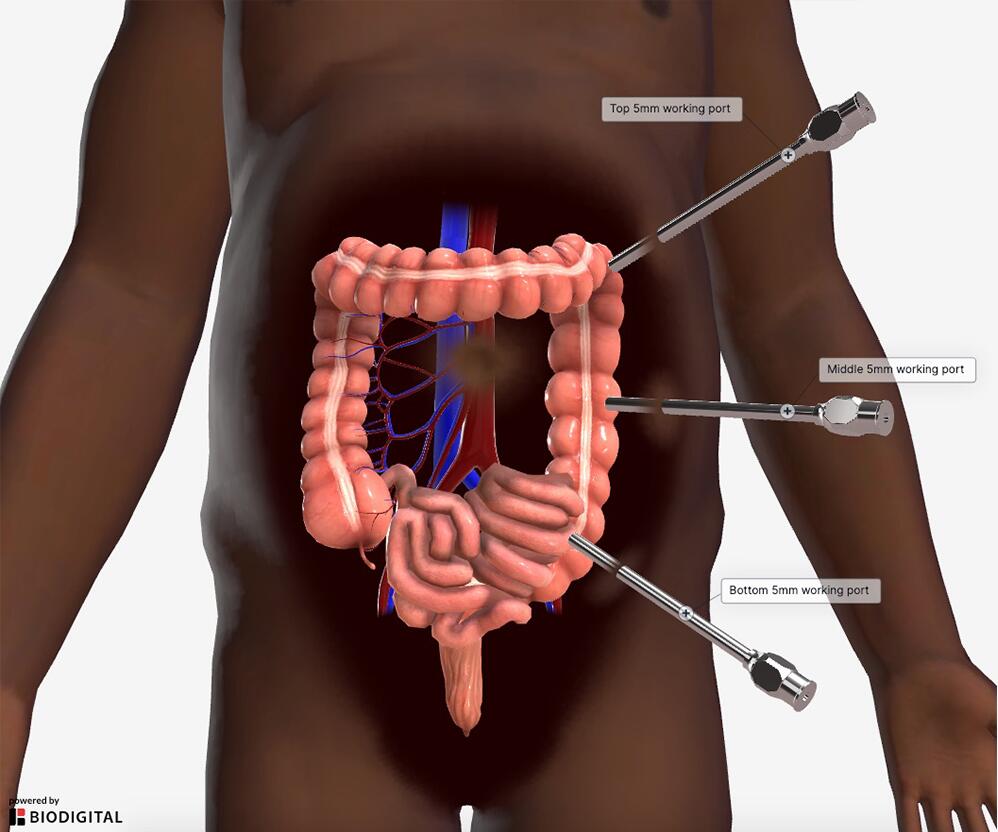
Common port placement
- Arrange ports thoughtfully in case conversion to hand assisted or open case will be required.
- Must know tumor location prior to starting the case for proper trocar placement.
- Generally, two to three 5 mm ports and one 12 mm port are used.
- These factors/decisions will affect trocar placement.
- Decide if vascular pedicles are stapled or energy is used.
- Decide intracorporeal or extracorporeal anastomosis.
- Colon extraction site.
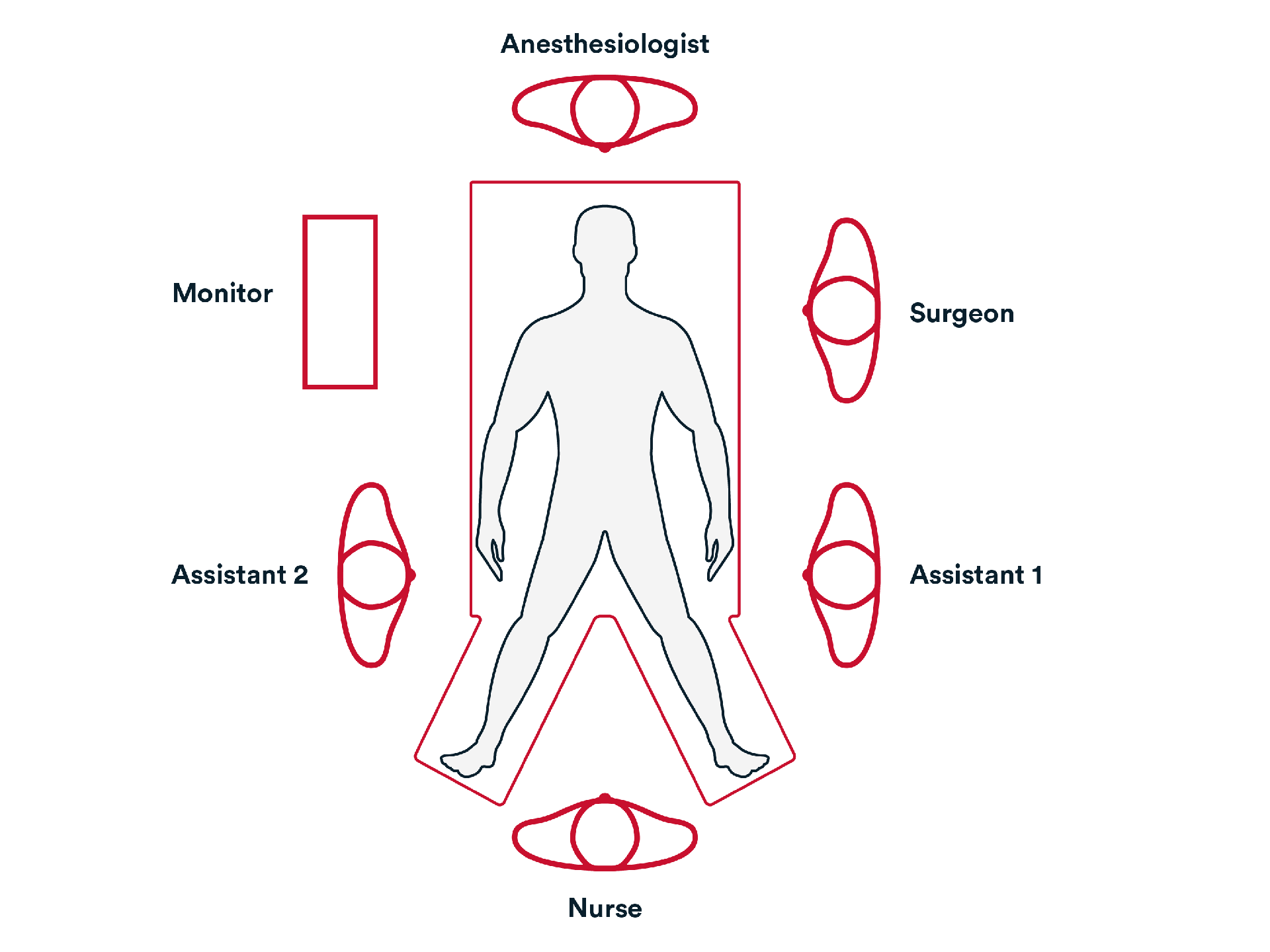
Common room setup
- The surgeon is usually on the patient’s left side with the assistant.
- Monitor is opposite from the surgeon.
- Recording device is available.
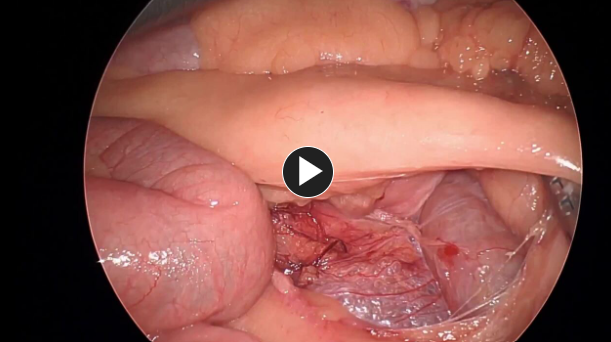
- Explore the abdominal cavity, assessing the liver and peritoneal surfaces.
- Take down any adhesions.
- Identify duodenum.
- Identify right ureter.
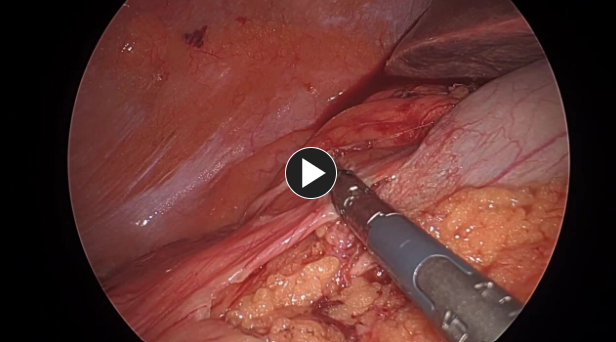
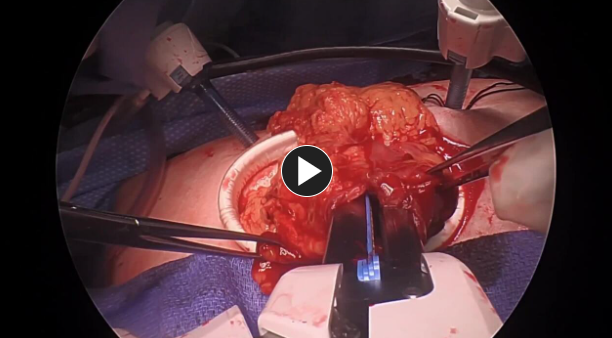
- Ensure a complete specimen with intact mesocolic envelope containing all lymph nodes, extract specimen.
2. Repair
- Transect distal ileum proximal to the ileocecal valve, using a stapling device, such as PROXIMATE™ Linear Cutters, and ensuring adequate blood supply to the remaining ileum.
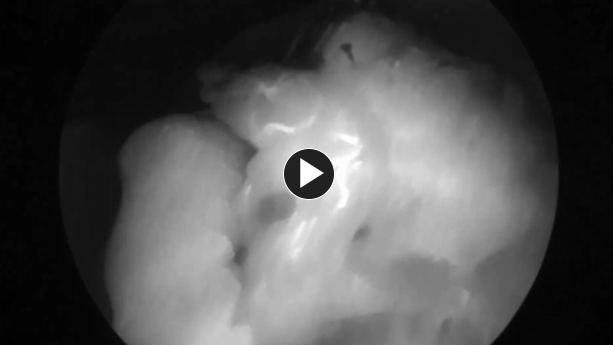
- Transect the proximal end of the right transverse colon, using a stapling device such as PROXIMATE™ Linear Cutters, and ensure adequate blood supply to the remaining colon by utilizing laser camera and ICG.
- Perform a side to side or end to side anastomosis, using a stapling device such as PROXIMATE™ Linear Cutters.
- Check the anastomosis for bleeding and leakage.
- Close the common enterotomy using a stapling device or suture such as Monocryl™ Plus Antibacterial suture or STRATAFIX™ Spiral MONOCRYL™ Plus Knotless Tissue Control Device and reinforce the staple line intervention if applicable.
3. Closure
- Generally, a closing tray and new gown and gloves are used to lower surgical site infection.
- Subcuticular layer and skin are closed using synthetic absorbable monofilament, such as Monocryl™ Plus Antibacterial suture, and a topical skin adhesive such as DERMABOND PRINEO™ Skin Closure System or any appropriate dressing.
- Inject wound with a local anesthetic.
Potential complications include but are not limited to:
- Surgical bleeding
- Staple line Leak
- Wound infection
- Ileus
- Urinary retention
Post-operative Patient Care
Typical recommendations for post-operative care may include, but are not limited to, any of the following:
- Typical discharge instructions consist of pain management.
- ERAS protocol such as early feeding, ambulation, remove foley catheter, non-narcotic pain control.
Additional resources

Access our on-demand GYN video library
Looking for more? Explore procedural videos and webinars from global experts

Energy Academy
This program offers concise learning to understand monopolar, bipolar, and ultrasonic energy modalities.