Bob Kiaii, MD
Mitral Valve Repair (MVR)
Procedure Overview
The mitral valve repair procedure treats diseases affecting the mitral valve, through which blood from the left atrium enters the left ventricle. If the mitral valve can't be repaired, surgery may be needed to replace the valve. In this procedure, a surgeon removes the mitral valve and replaces it with a mechanical valve, or a valve made from cow, pig or human heart tissue (biological tissue valve).
INDICATIONS:
- Stenosis: When calcium or other deposits build up on the valve, the valve opening become narrowed, inhibiting the flow of blood out of the ventricle.
- Regurgitation: The valve does not close completely, causing the blood to flow
backward into the left ventricle at the end of systole.

Pre-operative Patient Care
Typical recommendations for pre-operative care may include, but are not limited to, any of the following:
- Directed History & Physical Exam
- Laboratory Testing - CBC
- Laboratory Testing – Comprehensive Metabolic Panel
- Laboratory Testing – Coagulation Profile
- P2Y12 Test
- Preoperative Carotid Ultrasound Study
- Preoperative Pulmonary Function Test
- Echocardiogram – TTE and TEE
- Cardiac Catheterization – Right and left Heart
- CT scan
Prep & Patient Positioning
Prep
- Femoral arterial access is sometimes obtained when radial artery monitoring is a concern.
Common patient positioning:
- The most common position used for cardiovascular procedures is the supine position. This type of position allows the best possible surgical access to the chest cavity.
- For mitral valve repair, the anterior thorax is exposed with the patient in a supine position.
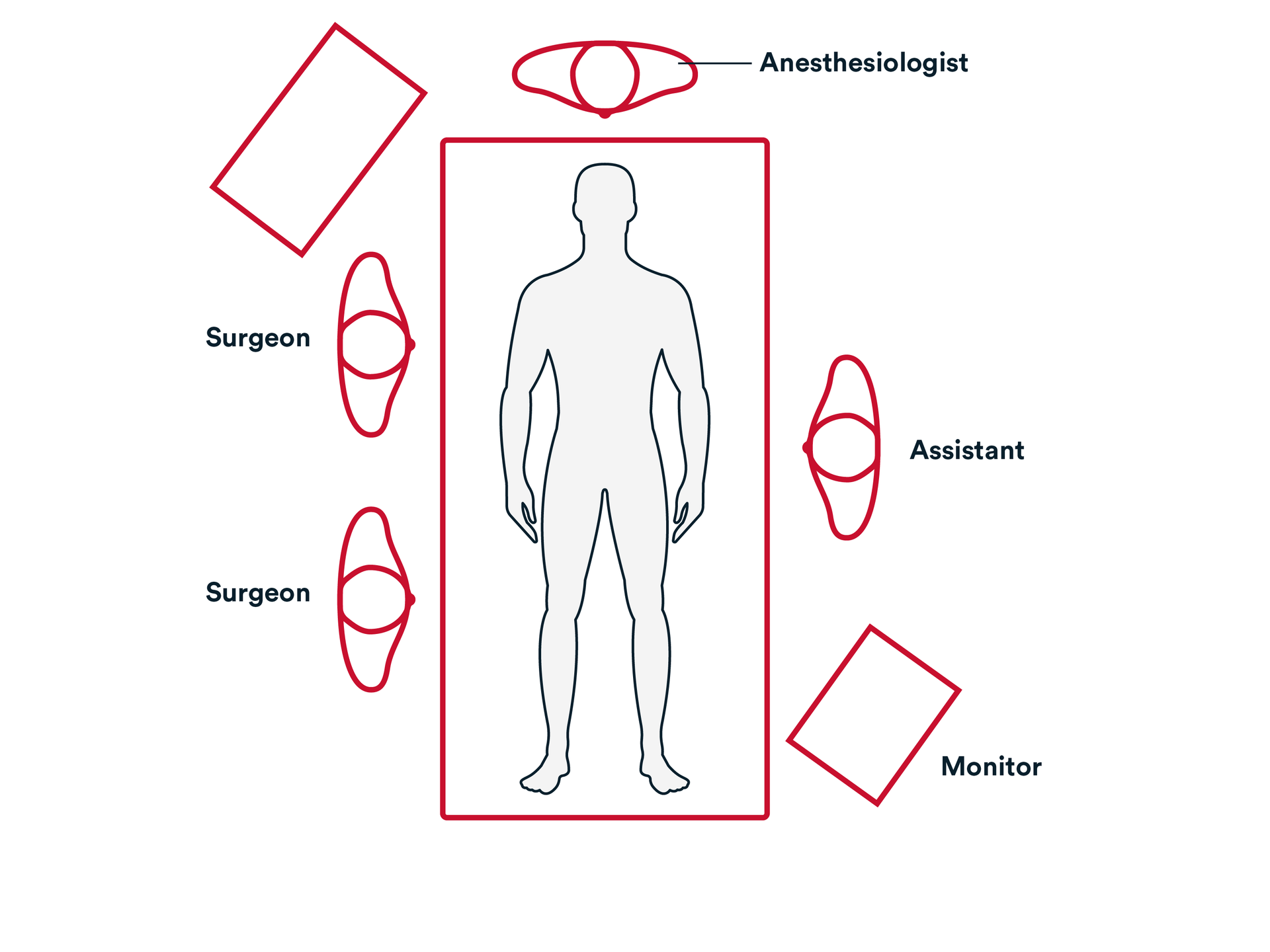
Common room setup
- The surgeon is almost always on the right side of the patient.
- Assistant on the left side.
- Bypass machine is usually close to the patient and can be on either side.
- Monitor that is positioned so the surgeon can see the hemodynamics during the procedure.
- Transesophageal echocardiogram machine is at the head of the patient.
Operative Steps
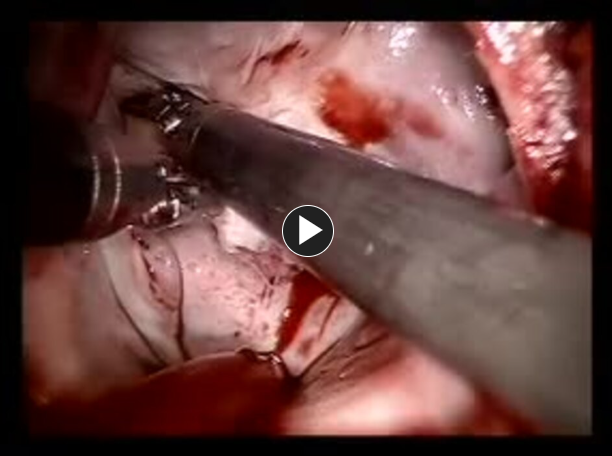
1. Access
Sternotomy:
- Skin incision is commonly made in the midline from jugular notch to xyphoid.
- NOTE: more advanced surgeons may choose to reduce the size of the incision, particularly at the top.
- Cell-saver suction is utilized to retrieve any blood loss during the procedure.
- Generally, at the sternal notch staying on the bone with the bovie cauterization and then using blunt dissection with a finger to palpate behind the upper manubrium to confirm that the space is clear. Similar blunt dissection at the xyphoid.
- A sternal saw is used to open the entire length of the sternum from sternal notch to xyphoid process, staying in the midline of the sternum.
- Bleeding from the sternal marrow and periosteum is commonly controlled to avoid ongoing oozing throughout the procedure. A topical absorbable hemostat such as SURGICEL™ FIBRILLAR Absorbable Hemostat can be applied to the sternal edges and bolstered with a sterile drape and the retractors.
Cannulation:
- The pericardium is opened from the diaphragm to its reflection at the upper ascending aorta, and the heart is exposed.
- NOTE: The upper pericardium is frequently covered in fatty tissue and remnants of the thymus gland. This can be a source of ongoing bleeding.
- Usually, 2-0 silk pericardial sutures are placed to retract the pericardium and expose the heart and great vessels.
- Arterial Cannula is placed.
- Venous Cannula is placed – Bicaval cannula (superior and inferior vena cava).
- Retrograde Cardioplegia Cannula may be placed as needed.
- NOTE: Retrograde Cardioplegia cannula is usually placed in more complex procedures
Arresting the Heart:
- An aortic cross clamp is applied across the aorta between the aortic cannula and the aortic root needle cutting off the flow of blood from the aortic cannula to the heart.
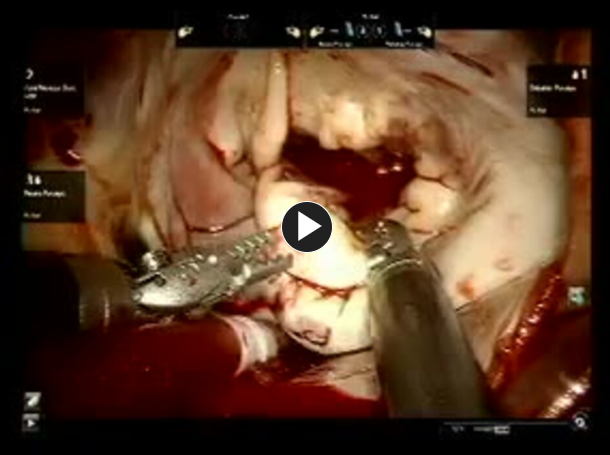
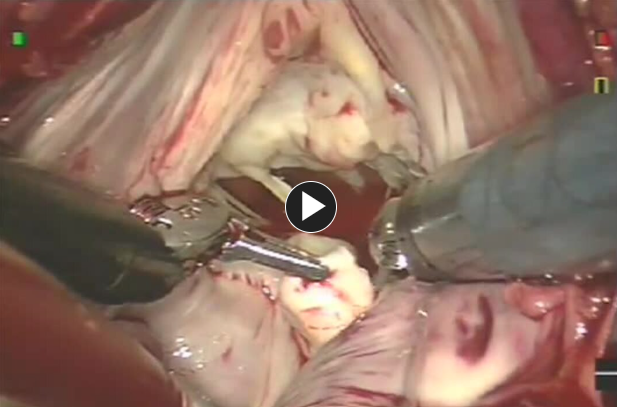
2. Repair
Accessing The Mitral Valve:
- The left atrium is entered through the interatrial (Sondegaard) grove.
- Left atrial Retractor frequently placed to pull up the roof of the atrial wall to expose the mitral valve.
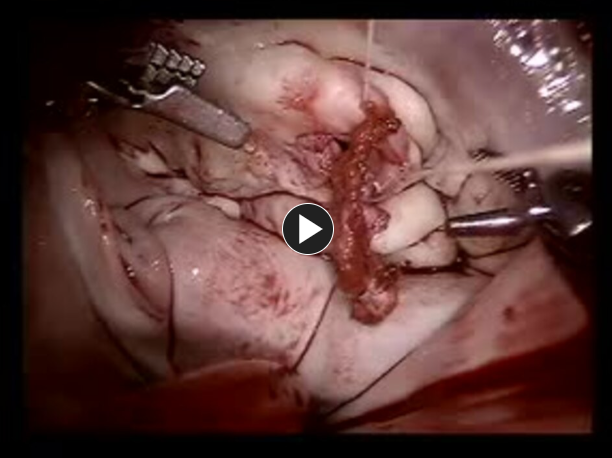
It is Important to take caution to avoid Systolic Anterior motion of the valve (SAM).
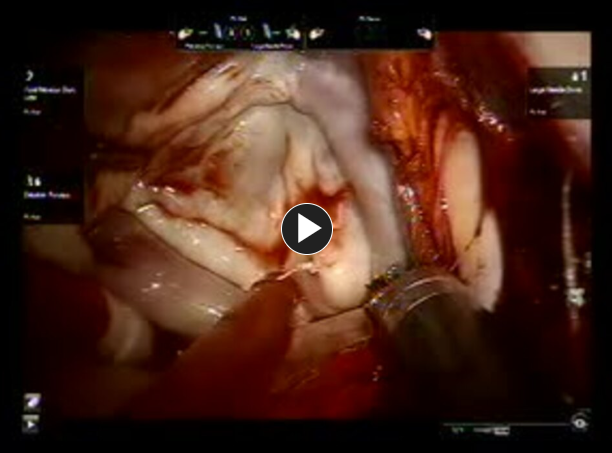
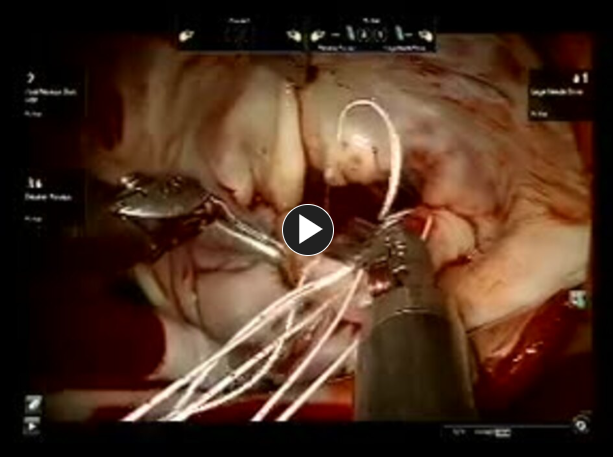
A suture guide is frequently used to organize the sutures.
The valve sutures are then placed through the annuloplasty ring or band.
The annuloplasty ring and band is lowered down onto the annulus. It is important to confirm that the ring and band is well seated on the native annulus.
The mitral valve is inspected for competency.
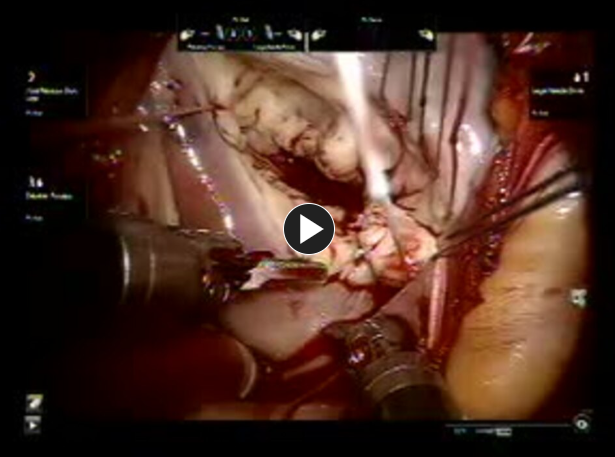
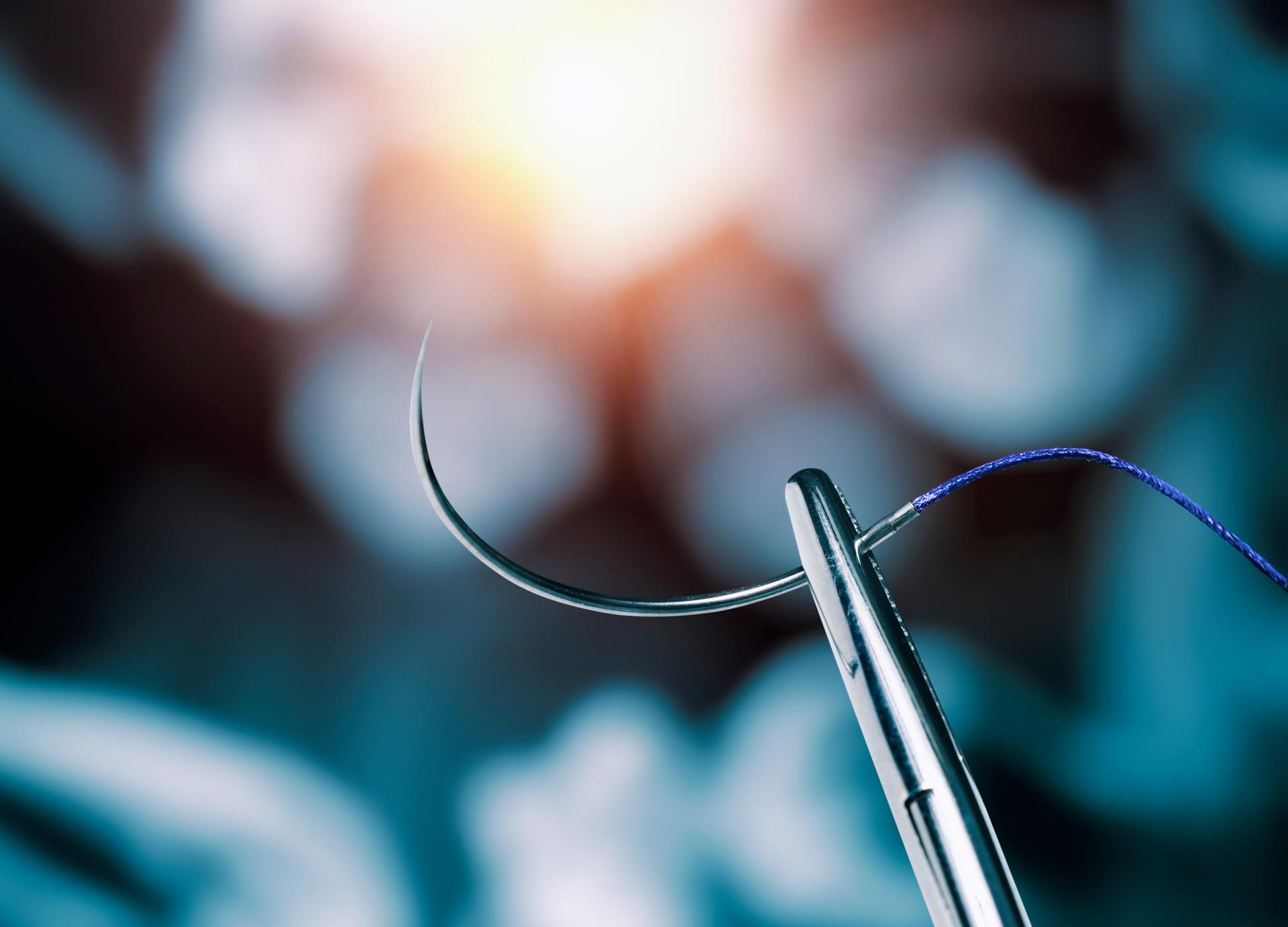
The left atrium is closed with a continuous running non-absorbable polypropylene suture, such as Prolene™ Polyopropylene suture (usually in two layers).
The left atrium is deaired by inflating the lungs.
The Aortic root vent is attached to suction.
The cross clamp is removed.
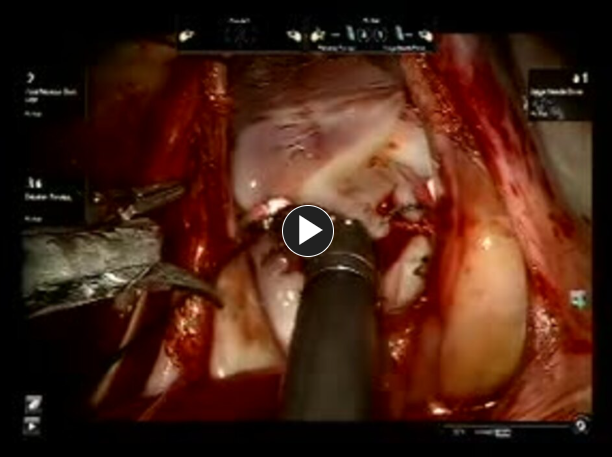
Preparing to disconnect from CPB:
- Once the cross clamp is removed blood flow to the coronary arteries is restored and spontaneous heart rhythm usually returns.
- Temporary pacing wires and chest tubes are placed.
- If the heart does not spontaneously start the temporary pacing wires may be used.
- NOTE: It is important to visualize both lungs expanding while anesthesiologist begins ventilating the patient.
Discontinuing cardiopulmonary bypass and cannulation :
- Once there is an adequate rhythm with reasonable contraction of both ventricles and the both lungs are being ventilated, the patient is ready to be weaned from the heart-lung machine.
- When CPB has been discontinued, the venous cannula, retrograde cannula and aortic root needle is removed.
- During this time any blood volume remaining in the heart-lung machine is returned to the patient.
- The aortic cannula is removed.
3. Closure
Confirm that there are no areas of active bleeding. Consider placing topical absorbable hemostat such as SURGICEL™ FIBRILLAR Absorbable Hemostat - on the sternal edges prior to closing the sternum to minimize oozing from the lower sternal table and to utilize its bactericidal affects.
Proximal anastomoses and cannulation sites are inspected for bleeding / oozing.
Integrity of the bypass grafts is checked for twists or kinks.
The overall heart function is assessed.
The sternotomy retractor is removed.
A laparotomy pad is placed in the incision and chest wall is inspected for bleeding.
Sternal wires are placed starting from the top (manubrium), using Surgical stainless-steel suture.
The wounds are closed using synthetic absorbable monofilament, such as Monocryl™ Plus Antibacterial suture, or a knotless tissue control device, such as STRATAFIX™ Knotless Tissue Control Devices, and a topical skin adhesive such as DERMABOND PRINEO™ Skin Closure System or any appropriate dressing.
- STRATAFIX
- DERMABOND PRINEO
Post-operative Patient Care
Typical recommendations for post-operative care may include, but are not limited to, any of the following:
- Patient usually recover in ICU setting with continuous hemodynamic and EKG monitoring.
- Patients are assessed for bleeding from the chest tubes.
- Patients are sedated and on the ventilator for up to 24 hours, depending on condition.
- 24-48 hours post-surgery transferred to a monitored step down unit.
- Discharged 4-6 days post-surgery.
- Follow-up withing first 2-4 weeks, depending on surgeon practice.
Additional resources

Access our on-demand Cardiovascular video library
Looking for more? Explore procedural videos and webinars from global experts
SuturED
SuturED consists of e-modules covering topics such as suturing techniques and the science of tissue management