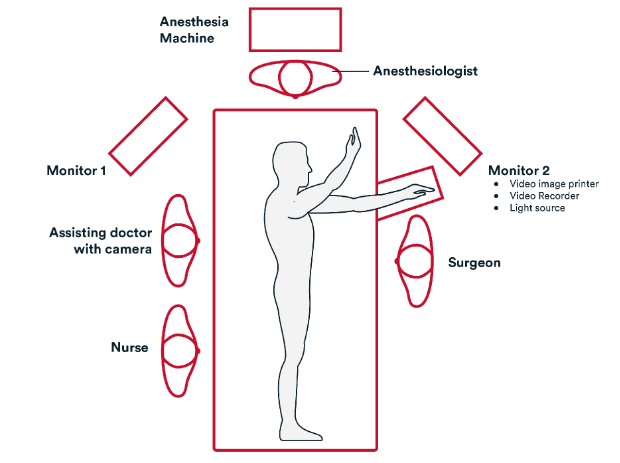
Prep & Patient Positioning
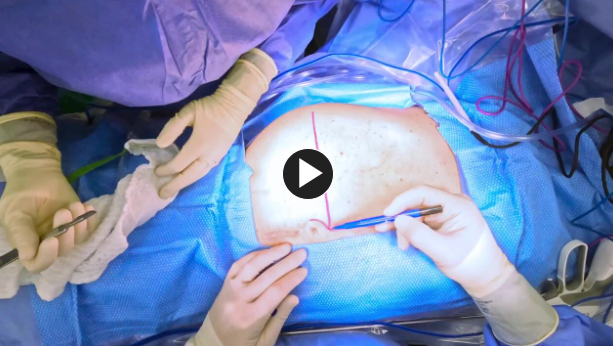
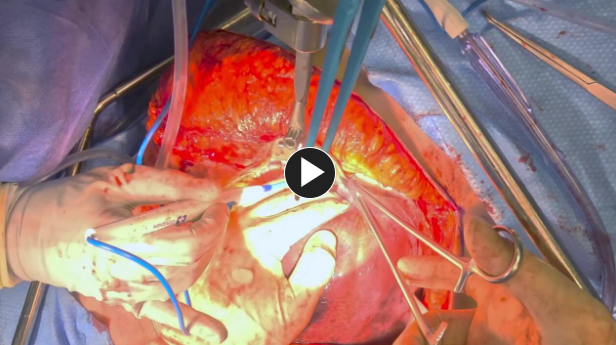
Operative Steps
2. Repair
3. Closure
- Resuspend the falciform ligament to minimize complication of liver torsion after hepatectomy.
- Place figure of eight synthetic absorbable suture such as #0 Vicryl™ Plus Antibacterial Suture to approximate the umbilicus prior closing the lateral incision.
- Fascia is closed in a running fashion using a synthetic absorbable suture such as #1 PDS™ Plus Antibacterial Suture.
- Skin closure is performed using a synthetic absorbable suture such as such as Monocryl™ Plus Antibacterial sutures and a topical skin adhesive such as Dermabond™ Prineo Skin Closure System.
Post-operative Patient Care
Typical recommendations for post-operative care may include, but are not limited to, any of the following:
- Remove foley catheter early if placed intraoperatively.
- ERAS protocol includes use of non-narcotic pain control with acetaminophen, gabapentin, and celecoxib as well as early and frequent ambulation and aggressive pulmonary toilet.
(Back to the top)
Additional resources