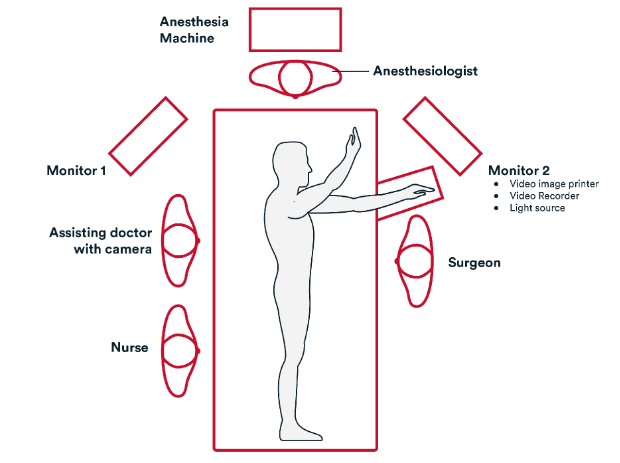
DISSECTING & DIVIDING BLOOD VESSELS
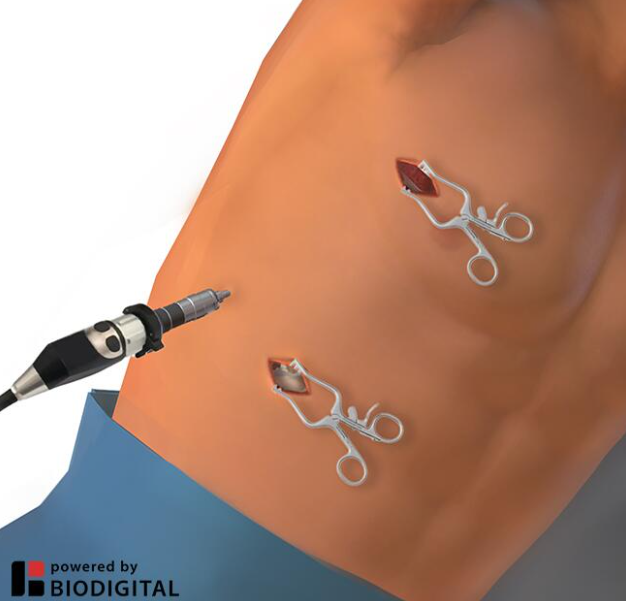
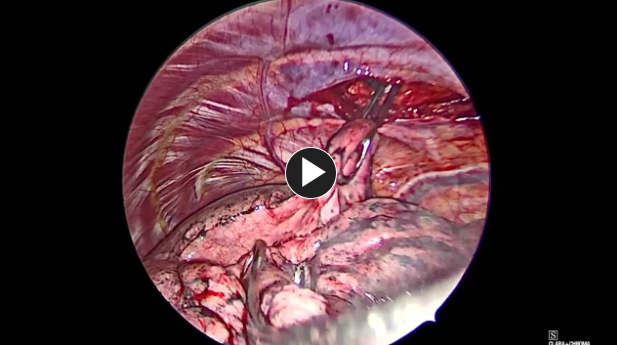
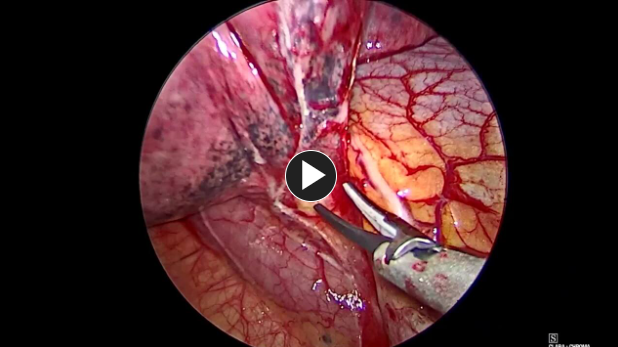
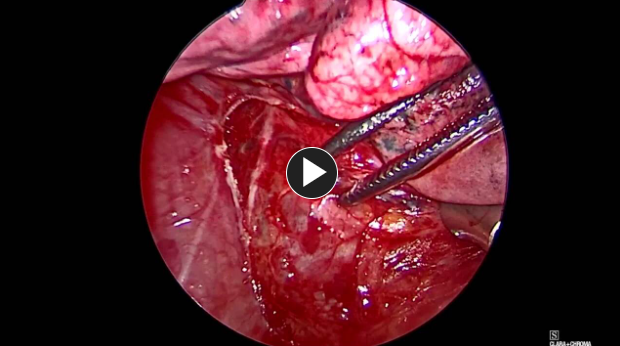
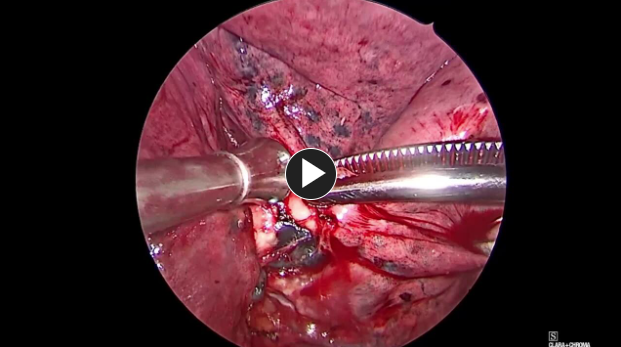
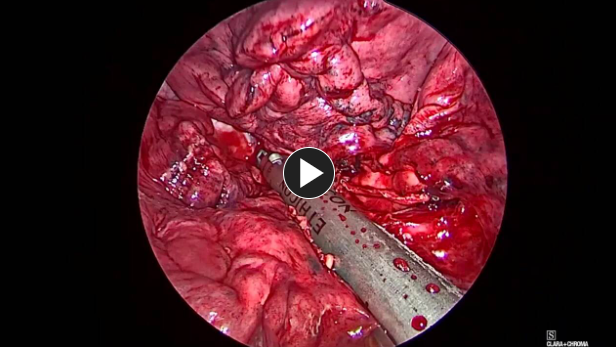
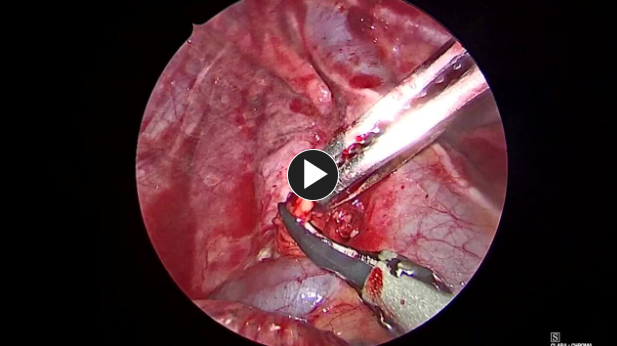
- For upper and middle lobes, dissect the upper and middle lobe pulmonary vein as it lies more anterior to the artery.
- For lower lobectomies, the inferior pulmonary vein is found at the base of the inferior pulmonary ligament.
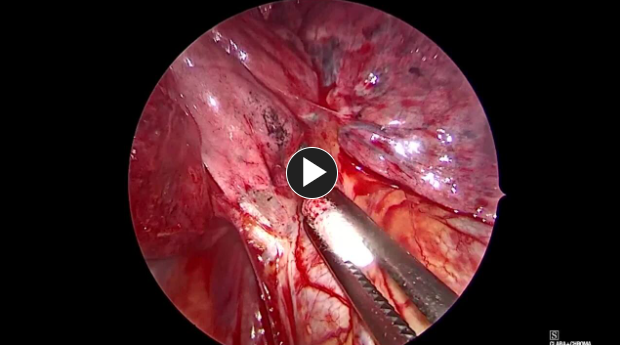
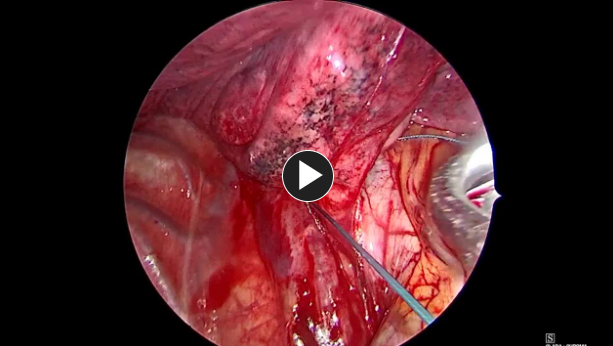
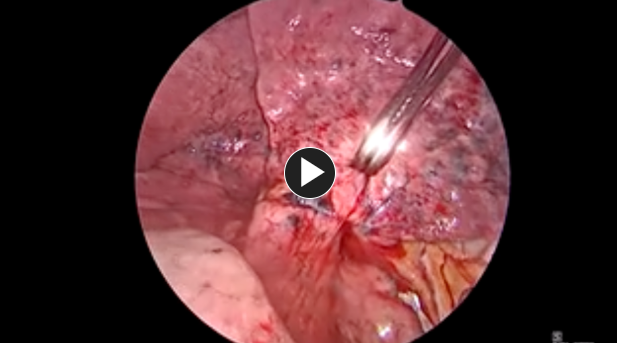
- Dissect and encircle the lobar bronchus with a suture or vessel loop.
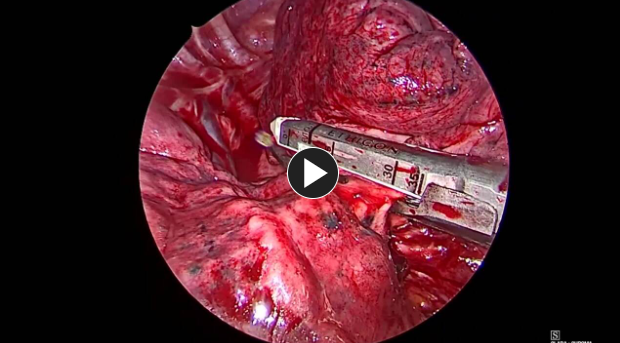
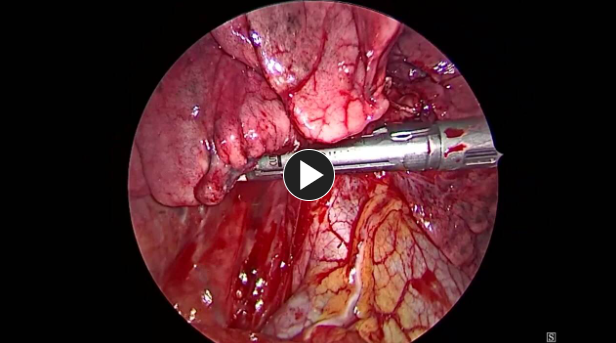
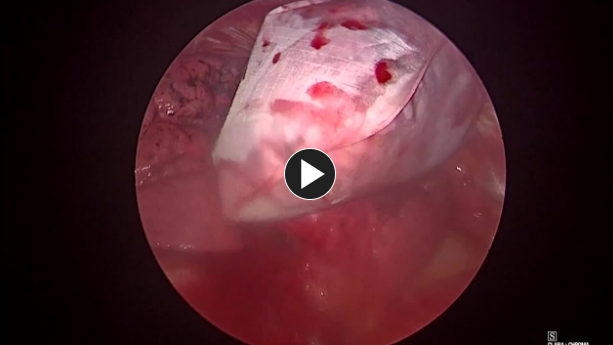
- Compress the lobar bronchus with the ECHELON 3000 stapler (Green load).
- Perform test ventilation to ensure no inflation of target lobe with adequate ventilation to remaining lung.
4. Closure
- Suction any remaining irrigation fluid.
- The deep and superficial subcutaneous tissue is closed with #2-0 Vicryl™ Plus Antibacterial sutures.
- Skin is closed with #4-0 PDS™ Plus Antibacterial sutures or Monocryl™ Plus Antibacterial sutures.
NOTE: “Debrief” with the O.R. team should verify the procedure performed, estimated blood loss, correct labeling of all pathology specimens, and anticipated postoperative needs.
Potential complications include but are not limited to:
- Air leak
- Bleeding
- Atelectasis
- Pneumonia
- Arrythmia
- Wound infection
Post-operative Patient Care
Typical recommendations for post-operative care may include, but are not limited to, any of the following:
- Remove foley catheter early if placed intraoperatively.
- ERAS protocol includes use of non-narcotic pain control with acetaminophen, gabapentin, and celecoxib as well as early and frequent ambulation and aggressive pulmonary toilet.
(Back to the top)
Additional resources