2. Repair
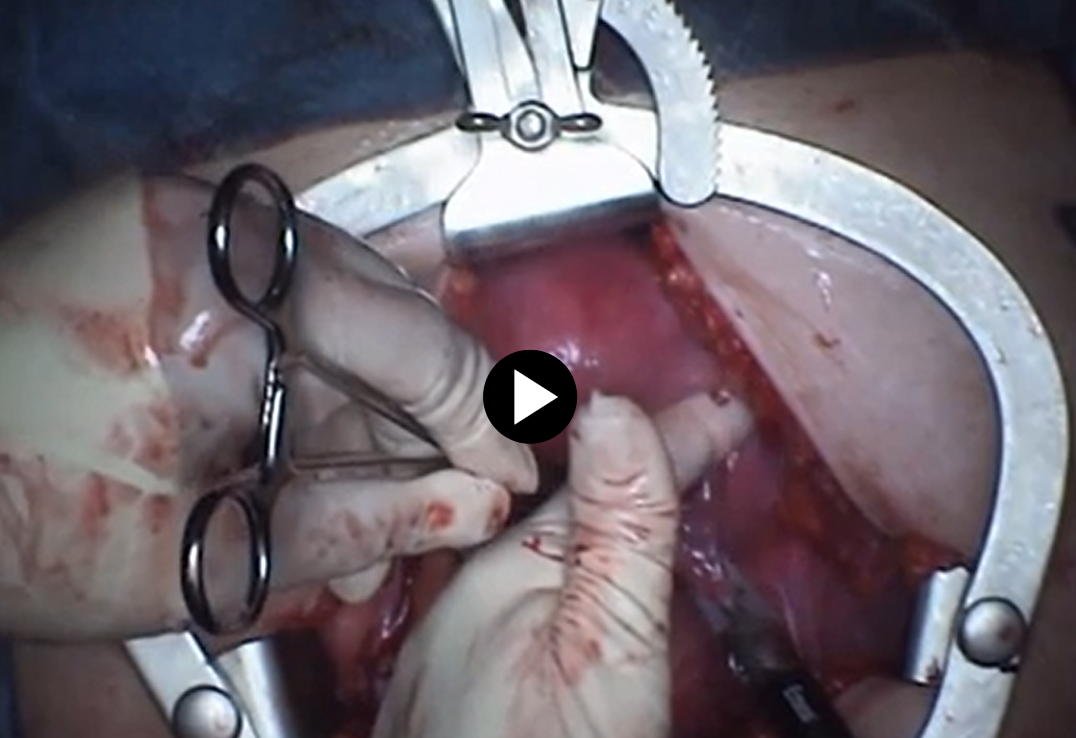
- The anterior bladder peritoneum is incised with scissors and the bladder is pushed down with the sponge stick forceps. Broad ligament is pushed forward with the surgeons’ fingers.
4. Abdominal Wall Closure
Post-operative Patient Care
Typical recommendations for post-operative care may include, but are not limited to, any of the following:
- Patients should improve each day postoperatively, temperature greater than 100.4, and increasing abdominal pelvic pain not relieved by
- Typical discharge instructions consist of medications for pain management and bowel regularity, diet, and activities, clinic follow-up in 2 weeks.
- Most patients will be discharged the same day or 23 hours stay.
Patients are recommended to follow any nutritious diet that they can tolerate and generally first try liquids and foods that may be easily digestible. - Patients are encouraged to ambulate early (with assistance if needed) even on the day of surgery to reduce deep vein thrombosis (DVT) risk.
- Generally, patients are asked to be active as they can tolerate but limit strenuous activities.
Additional resources