George Crawford, MD
Ventral Hernia Repair - Small Umbilical Hernia without Mesh

Procedure Overview
Ventral hernias can be categorized as incisional, umbilical, or epigastric. Small ventral hernias can be repaired by excising the hernia sac and closing the fascia with suture, without using a mesh.
INDICATIONS:
- Ventral hernia repair may be indicated to prevent or address symptoms related to the hernia such as pain, acute incarceration, enlargement, and skin problems.
- The most common sites for ventral hernias are the navel (an umbilical hernia) and the site of a previous abdominal procedure (incisional hernia).

Pre-operative Patient Care
Typical recommendations for pre-operative care may include, but are not limited to, any of the following:
- CT Scan with PO and IV contrast.
- Cardiopulmonary evaluation as needed.
- Anesthesiology consultation as needed.
- Nothing by mouth for 6 hours before surgery.
- Prophylactic antibiotics for patients with comorbidities such as heart disease, diabetes, previous history of colon or bowel surgery.
- BMI greater than 40 and smoking are relative contraindications.
Prep & Patient Positioning
Common patient positioning:
- A supine position with the arms tucked at the patient's sides, for patients with midline hernias.
- A lateral decubitus or modified lateral decubitus position, for hernias of the flanks or posterior abdominal wall.
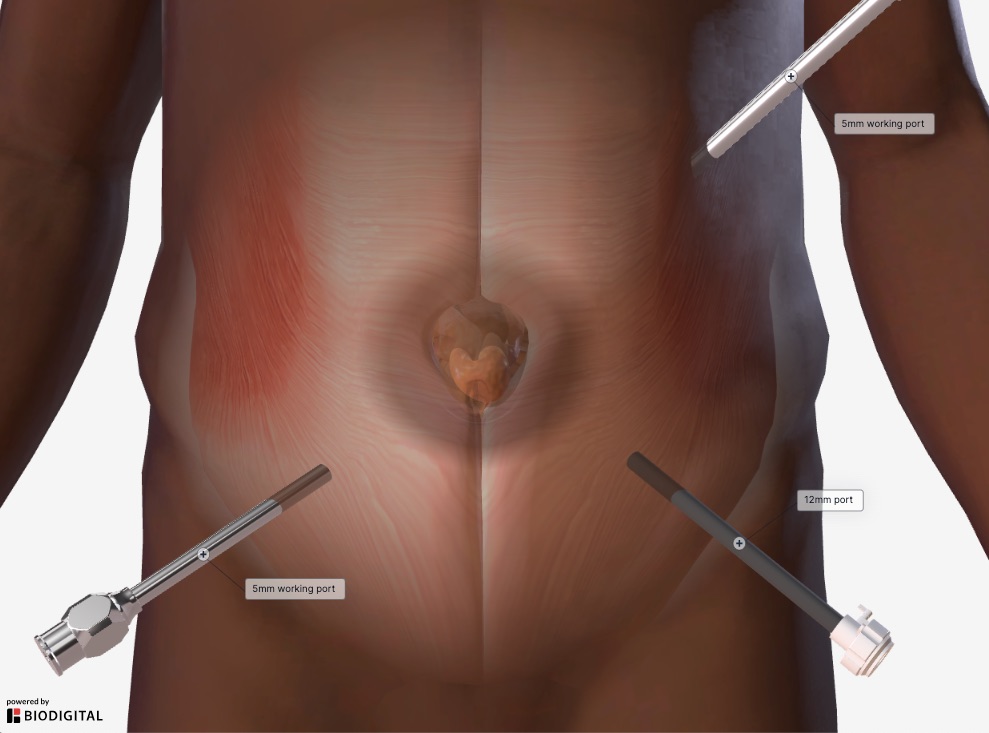
Common port placement
- The location of initial abdominal access (primary port placement) for laparoscopic ventral hernia repair is typically as far from the hernia defect and prior laparotomy incisions as possible.
- A Veress needle, open Hasson technique, or optical trocar entry may all be used for primary port placement. The specific technique used should be primarily based on the surgeon’s experience and outcomes with the technique and take into consideration the patient’s surgical history and anatomy.
- Secondary port placement is generally performed under direct vision and placed as lateral from the hernia defect as possible to allow the surgeon to work in an ergonomically favorable position.
Operative Steps
1. Access
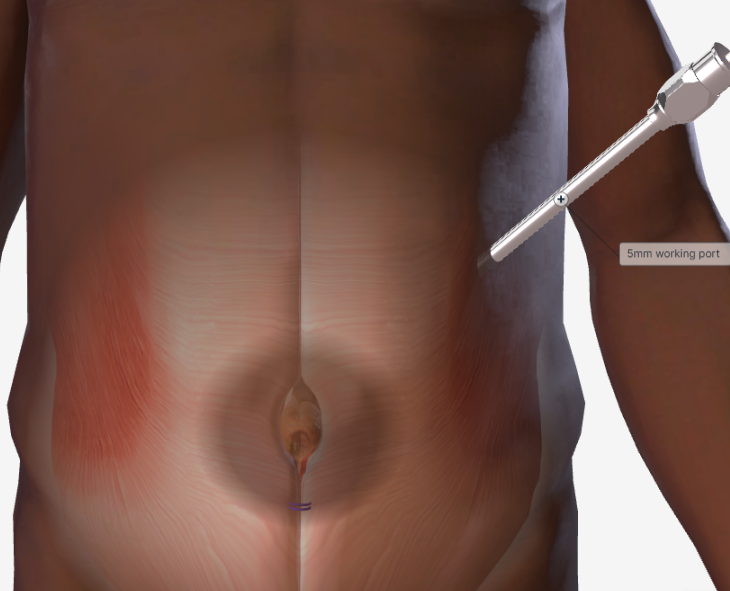
- Access is generally obtained through an incision in the left upper quadrant. Usually, a 5 mm trocar is used to enter the abdomen if laparoscopic assistance is needed.
- The abdomen is insufflated to visualize the ventral hernia defect.
- NOTE: Once visualized and safe, an incision can be made over the ventral defect. If intra-abdominal contents cannot be reduced under direct visualization, then additional 5 mm trocar can be placed to facilitate.
2. Repair
- An incision is made over the ventral hernia. The subcutaneous tissue is dissected.
- The hernia sac is dissected out bluntly and exposed.
- Once completely exposed, the hernia sac is excised at the base of the fascial defect. The fascia is exposed circumferentially around the defect. For small defects, suture such as Vicryl™ Plus Antibacterial suture, Prolene™ Polypropylene, or Ethibond EXCEL™ Polyester may be used to re-approximate the facia. For larger defects, a suture passer technique may be utilized.
- If this is an umbilical hernia, and the umbilicus has been mobilized away from the facia, it may be reapproximated, such as a size 0-Coated Vicryl™ Plus Antibacterial suture.

3. Closure
- The trocars are removed. The wounds are closed using synthetic absorbable suture, such as Monocryl™ Plus Antibacterial suture, and a topical skin adhesive such as DERMABOND ™ PRINEO™ Skin Closure System or any appropriate dressing.
Post-operative Patient Care
Typical recommendations for post-operative care may include, but are not limited to, any of the following:
- The patient is out of bed, ambulating, with appropriate pain control.
- Diet is advanced as tolerated, with plans for discharge on postoperative day 0 for routine umbilical hernia.
- Lift nothing heavier than 25 lbs. for two weeks.
- Resumption of normal activity, minus lifting restrictions, occurs within 1 day following the procedure.
- Discharge instructions consist of pain management, instructions on the future signs and symptoms indicating potential complications (see below), and an office appointment in 1 weeks’ time.
Potential complications may include but are not limited to, any of the following:
- Nausea, vomiting, or severe coughing spells.
- Fever greater than 101.5 degrees.
- Redness or Erythema.
- Swelling or drainage from the previous hernia site.
- Change in amount of drainage or the color of the drain output if a drain is present.
Additional resources

Access our on-demand Hernia video library
Looking for more? Explore procedural videos and webinars from global experts
HERNIAcademy
Offering comprehensive education about the treatment of inguinal and abdominal hernias


